The degeneration of endometriosis and malignancy
Nouvelles recommandations HAS pour les bonnes pratiques en imagerie de l'endometriose
14h00 - Amphithéâtre Havane
First topic is ‘polypoid endometriosis’, a distinct form of endometriosis, is rare but important because it might be mistaken for a neoplasm on imaging, intraoperative, and pathologic examination. As a clinical characteristic, patients with polypoid endometriosis are over 50 years of age, in contrast to usual endometriosis, which typically affects women of reproductive age. Although multiple sites tend to be involved in the same patient, the most frequent sites are the rectum and sigmoid colon, followed by the ovary. Macroscopically, it shows exophytic or polypoid tumor-like masses; it sometimes accompanies variable degrees of cystic change and hemorrhage. Microscopically, the polypoid masses comprise an admixture of endometriotic glands and stroma. Reflecting the macroscopic and microscopic appearance, MRI shows a high signal intensity mass with a peripheral hypointense rim on T2WI and prominent enhancement similar to that of the endometrium. Because this is benign endometrial tissue, both DWI and ADC map show high signal intensity. Those specific MR image findings will
Second topic is decidualization of endometrial tissue in endometrioma. During pregnancy, hormonal changes induce the uterine endometrium to thicken and to transform to decidua with hypertrophy of the endometrial stromal cells, known as decidualization. Similar histological changes can occur within ectopic endometrial tissue. Then, endometriotic cyst with decidualization can show mural nodules on US and MRI, mimicking endometriosis-associated ovarian carcinoma (EAOC). Although decidualization is a transient condition that disappears during follow-up, it can be removed surgically when misdiagnosed as a tumor with solid portion. Therefore, proper diagnosis of this condition is clinically important. Several characteristic MRI findings are known. On T2WI, decidualization is recognized as linear, broad-based nodular, or polypoid structures with high signal intensity similar to that of placental tissue. It also shows high signal intensity both on DWI and ADC map. Regarding the differentiation of decidual change from EAOC, heights of the mural nodules measured from the cystic wall or the septum were less than 11 mm in endometriotic cysts with decidualization (no overlap with carcinomas).
The main topic is EAOC. Why endometrotic cyst have to be followed by US or MRI? The most critical problem is emergence of carcinoma derived from endometriotic cysts. Although it is rare (approximately 1%), the relative risk of developing ovarian cancer is up to 4.2 times greater for women with endometriosis than for the general population. Most frequent tumor derived from endometriotic cysts are clear/endometrioid carcinoma. Less frequently, benign and borderline seromucinous tumors are observed. Each of the tumors shows the different carcinogenesis that ovarian endometrioid carcinoma develops under unopposed estrogen environment {Mandai, 2009 #2203}. In contrast, clear cell carcinoma arises in the condition of oxidative stress from free-iron of menstrual blood accumulating in the cystic fluid causing the DNA damage, resulting in the cancer development {Mandai, 2011 #2204}.
Early detection of malignant transformation is important because clear cell carcinoma is chemotherapy-resistant. Of the three key MRI findings for EAOC diagnosis, the most sensitive finding is the emergence of enhanced mural nodules within the ovarian endometriotic cyst. Although 97% EAOC accompanies enhanced mural nodules, it should be noted that a certain amount of benign lesions also show enhanced mural nodules. The second key finding is increased tumor size. Kobayashi et al. reported ‘9 cm’ or greater diameter of endometriotic cyst as an independent predictive factor for future development of ovarian cancer. The last finding is a lack of T2-shading, which might be induced by dilution of hemorrhagic fluid by secretion from a malignant tumor. T2-Shading was present in 81.3% in a benign condition, in contrast to 33.3% in EAOC. From investigations of longitudinal change of the same endometriotic cyst by Nishio et al., 20% of benign endometriotic cysts also showed a change of SI from low SI to high SI on T2WI during follow up. The lack of shading might be an alarming finding, but not specific to EAOC.
After listening to this ‘Endometriosis’ session, you will be able to confidently interpret MRIs for suspected endometriosis and write more detailed and precise reports for the gynecologists and patients.
QUIZ: Which is the endometriosis-associated ovarian carcinoma?
You will know the answer at the lecture !
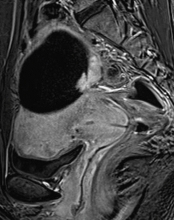
Case 1: CE-T1WI, subtraction
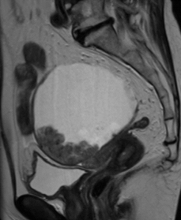
Case 2: T2WI
